Understanding Antidepressants
It’s nearly impossible to fully understand the relationship between antidepressants and alcohol unless you know exactly how antidepressants work.
Antidepressants are medications used to manage symptoms of depression, anxiety, and other mental health issues. These medications are prescribed to lift your mood and help you find a more balanced emotional state. There are different types of antidepressants, each having a different effect.
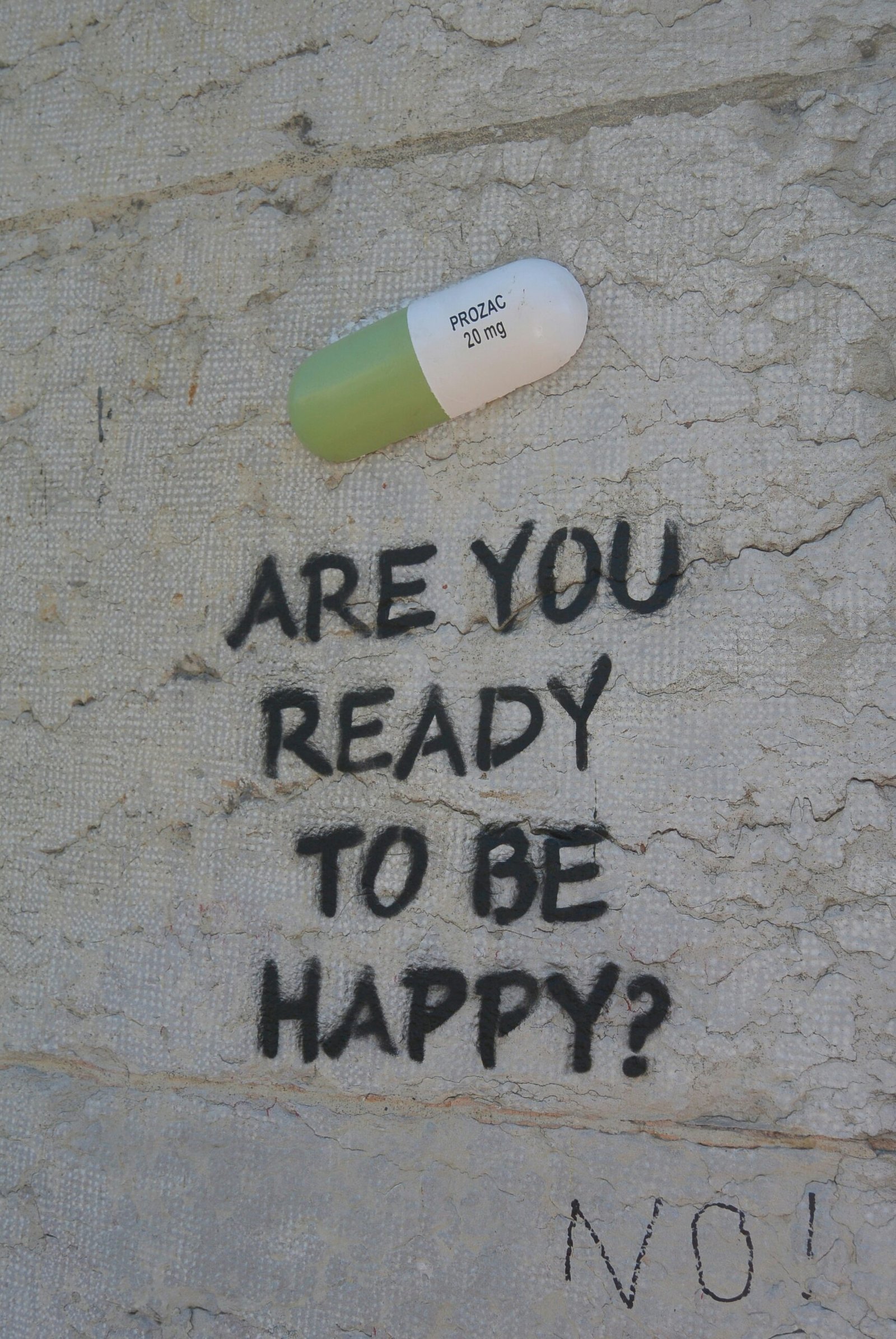
One of the most commonly prescribed types is selective serotonin reuptake inhibitors (SSRIs). These medications increase the levels of serotonin in the brain, a neurotransmitter responsible for mood regulation. Some common SSRIs include fluoxetine, sertraline, and escitalopram. They’re often recommended as a first choice for treatment because they tend to have fewer side effects and are easy to use.
Another important group is serotonin-norepinephrine reuptake inhibitors (SNRIs). These work by boosting levels of both serotonin and norepinephrine in your brain. Based on the presenting symptoms, Doctors can add SNRIs if they find that SSRIs aren’t enough to help with your symptoms. Examples of SNRIs include venlafaxine and duloxetine.
There are also tricyclic antidepressants (TCAs), which are an older class of medications. While they can be effective, they’re prescribed less frequently because they often come with more side effects. TCAs change the balance of different neurotransmitters in your brain, but they might lead to issues like weight gain and sedation.
While antidepressants can make a significant difference in how you feel, it’s better to be aware of the potential side effects. Issues like nausea, weight gain, insomnia, and sexual dysfunction can occur. Continuous medical support is necessary when starting antidepressants, as your doctor will check in on how you’re responding to the medication, and adjust your dosage accordingly.
The Role of Alcohol in Mental Health
Alcohol is a central nervous system depressant. Initially, you may feel relaxed or euphoric, but in the long run, it can slow down brain activity and lead to negative effects on your mood. Many people turn to alcohol to cope with anxiety and depression, but this often creates a cycle where drinking worsens those very symptoms.
Research shows that alcohol disrupts the balance of neurotransmitters in your brain, especially serotonin and dopamine, which are crucial for mood regulation. If you drink excessively, you might find that your feelings of sadness and anxiety increase. Over time, this can raise your risk of developing more severe mood disorders, illustrating how alcohol use can deteriorate your mental health.
Furthermore, the social settings around alcohol consumption can shape how you view drinking as a coping mechanism. In many cultures, drinking is considered a customary part of socializing or celebrating. This can make it easy to overlook problematic drinking behaviors, complicating your relationship with alcohol and mental health.
Potential Risks of Mixing Antidepressants and Alcohol
When you’re undergoing treatment with antidepressants, drinking alcohol can pose serious health risks. It’s easy to ignore the potential risks and harmful effects produced by the potential interaction between these two substances, but failing to do so will only take a devastating toll on your health.
Right off the bat, alcohol reduces the effectiveness of your antidepressants. When you mix alcohol with antidepressants, it might interfere with how your body processes these medications, prolonging and even deteriorating the symptoms you’re trying to manage.
Since alcohol is a central nervous system depressant, it also intensifies common side effects of antidepressants, like drowsiness and dizziness. This can become particularly hazardous during daily activities that require full attention, such as driving or operating machinery, as the combination can negatively impact your judgment and motor skills. You might also find that drinking leads to increased anxiety or mood swings, which goes against the goals of your treatment.
Another important factor to consider is the risk of developing a dependence on both alcohol and antidepressants. Alcohol may seem like a quick way to boost your mood, which can lead you to self-medicate when you’re feeling down or anxious. Over time, this can create a cycle where you feel you need to drink to feel better, making it harder to follow your prescribed antidepressant regimen. This interdependence can complicate your treatment and pose serious risks to your overall health and well-being.
Symptoms to Watch For
When you’re taking antidepressants, mixing them with alcohol can lead to a range of symptoms that signal a negative reaction. You must be aware of these warning signs, as they can have a significant impact on both your mental and physical well-being.
First, if you notice that your mental health symptoms are getting worse, this should raise a red flag. You might find that your feelings of anxiety, depression, or irritability become more intense. This can make your antidepressant treatment less effective, leading you to seek relief through alcohol, which often makes things worse.
Pay attention to any physical reactions as well. You might experience dizziness, nausea, or fatigue. These discomforts can be signs of increased sedation, especially if you’re on certain types of antidepressants, such as SSRIs or SNRIs. Mixing these medications with alcohol can also compromise your motor skills, making it harder to coordinate your movements and increasing your risk of accidents. If you experience any unusual physical reactions, it’s essential to seek assessment right away.
You might also observe changes in your behavior. This could include erratic decision-making or impulsive actions when you’re consuming alcohol alongside your medications. You could find yourself engaging in riskier behaviors or experiencing sudden mood swings. These shifts can signal that you’re struggling to manage your mental health while drinking. It’s crucial to keep a close eye on how you react and behave in these situations.
Overall, recognizing these symptoms early can help you take action. It may lead you to seek professional help or adjust your treatment plan. Being aware of how antidepressants and alcohol interact is key to ensuring your safety and achieving the best possible outcomes for your mental health.
Guidelines for Responsible Alcohol Use
Navigating the consumption of alcohol while you’re on antidepressants can be quite tricky, and it’s important to approach it thoughtfully. First, you should be aware that mixing alcohol with antidepressants can sometimes worsen symptoms of depression and anxiety or amplify the side effects of your medication. That’s why being mindful about how much you drink is essential.
Moderation is key for you. Generally, it’s suggested that women limit themselves to one drink a day, while men can have up to two. However, everyone’s body reacts differently to alcohol based on factors like your weight, metabolism, and the type of antidepressant you’re taking. Keeping a journal to track your experiences with alcohol might help you identify what works best for you over time.
In some cases, you might find that it’s better to skip alcohol altogether. If you have a history of substance abuse, struggle with managing your emotions, or have experienced strong side effects from your antidepressants, complete abstinence could be the safest option. It’s always a good idea to discuss your situation with your healthcare provider. They can help you weigh the risks and give you personalized advice on whether it’s okay for you to drink in moderation.
While you’re drinking, pay close attention to how you feel. If you notice any worsening symptoms of depression or anxiety, it’s worth reconsidering your drinking habits. Ultimately, being responsible about alcohol while on antidepressants means understanding your situation, committing to moderation, and keeping the lines of communication open with your healthcare team.
Alternatives to Alcohol for Coping
In navigating the complexities of life, many individuals may find themselves seeking methods to cope with stress, socialize, or enhance their mood. Alcohol has often been perceived as a quick solution; however, it can lead to detrimental health consequences, particularly for those on antidepressants. Hence, exploring alternatives to alcohol is imperative for fostering a healthier lifestyle.
Engaging in physical activities serves as an excellent alternative to alcohol for stress management. Exercise stimulates the release of endorphins, often referred to as “feel-good” hormones, which uplift mood and improve overall well-being. Whether it is running, swimming, or participating in group classes, physical movement can be an invaluable tool for tapping into one’s emotional health.
Another avenue to explore is creative hobbies. Activities such as painting, writing, or playing a musical instrument not only offer a productive outlet for emotions but also help in cultivating a sense of achievement and personal expression. These pursuits can foster connection with oneself and others while providing a fulfilling alternative to the temporary satisfaction derived from alcohol.
Practicing mindfulness and meditation has gained recognition as a powerful method for coping with stress and enhancing emotional resilience. Techniques such as deep breathing, guided imagery, and yoga can help individuals stay present, reduce anxiety, and improve their mood. These practices provide mental clarity and can become integral parts of a balanced lifestyle.
Lastly, forming supportive social networks that do not revolve around alcohol can significantly influence one’s emotional health. Surrounding oneself with individuals who share similar values promotes healthy interactions and emotional connections, alleviating the pressures often experienced in alcohol-centered social settings.
By embracing these alternatives, individuals can cultivate healthier coping strategies and, in turn, enhance their overall quality of life without relying on alcohol. The journey toward emotional well-being and social fulfillment is multifaceted, yet achievable through positive lifestyle choices.
Personal Stories and Testimonials
Every individual’s journey with mental health and substance use is unique, and personal stories often illuminate the challenges faced when antidepressants and alcohol intersect. Consider the experience of Mark, a 32-year-old man who suffered from depression for several years. Mark was prescribed an antidepressant that significantly improved his mood. However, he found himself resorting to alcohol on weekends, believing that it would enhance his social interactions and relieve stress. Over time, Mark noticed that the combination of alcohol and his medication hindered his progress, causing increased anxiety and disrupted sleep patterns. This realization prompted him to reassess his relationships with both substances, leading to an eventual commitment to sobriety while continuing his therapy.
On the other hand, Laura, a 28-year-old woman, presents a different perspective. She navigated her anxiety with the help of antidepressants while occasionally enjoying a glass of wine. According to Laura, it was a delicate balance; the initial effects of alcohol seemed to ease her tension. However, she soon recognized that even small amounts could lead to mood swings and exacerbate her symptoms. Her turning point arrived during a family gathering where, after a few drinks, she faced considerable emotional backlash, prompting her to seek help from her healthcare provider. This conversation led Laura to establish clearer boundaries around her alcohol consumption, enhancing her mental wellness while adhering to her treatment plan.
These testimonials represent just a fraction of the experiences shared by many individuals who find themselves contemplating the intricate relationship between antidepressants and alcohol. By shedding light on these personal stories, we emphasize the importance of self-awareness and open dialogue with healthcare professionals to navigate personal challenges in mental health management effectively.
Resources for Help and Support
Understanding the complexities surrounding antidepressants and alcohol is crucial for those navigating mental health and substance use issues. It is essential to seek professional help and support when confronted with these challenges. Numerous resources are available to assist individuals in need, which can provide invaluable guidance and promote recovery.
One of the most critical resources is contacting healthcare professionals, including psychiatrists, psychologists, and licensed counselors who specialize in mental health and substance use disorders. These experts are equipped to guide individuals through their treatment options and offer personalized care based on specific needs. Organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) provide a national helpline that can assist in locating local treatment facilities, support groups, and counselors.
Support groups such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) offer a network of peers who can share experiences and provide encouragement in a non-judgmental environment. These groups often focus on the intersection of substance use and mental health, promoting a holistic approach to recovery. Additionally, many local mental health organizations host support groups or therapy sessions that can foster a sense of community and understanding.
For educational purposes, websites like MentalHealth.gov and the National Institute of Mental Health (NIMH) offer valuable information on the effects of alcohol when taken with antidepressants, possible interactions, and coping strategies. These platforms aim to educate individuals and their families about the importance of informed decision-making regarding substance use in relation to mental health treatment.
In exploring these resources, individuals can improve their chances of finding the right support system while engaging with professionals trained in managing both antidepressant medication and alcohol use. Taking the first steps toward seeking help is instrumental in fostering recovery and well-being.
Conclusion: Making Informed Choices
In evaluating the intricate dynamics between antidepressants and alcohol, it becomes evident that a nuanced understanding is essential. Throughout this discussion, we have explored how alcohol can significantly interfere with the efficacy of antidepressant medications, potentially exacerbating symptoms of depression and anxiety. The consumption of alcohol while undergoing treatment with antidepressants can lead to myriad side effects, including increased drowsiness, dizziness, and impaired motor skills, complicating both the recovery process and daily functioning.
Additionally, it is important to recognize that the relationship between these substances is not merely pharmacological. Alcohol can alter mood and cognition, thereby counteracting the positive influence of antidepressants. This interaction suggests that individuals should maintain awareness of their drinking habits, particularly when they are prescribed these medications. Understanding the potential risks and consequences associated with combining alcohol and antidepressants can empower patients to make more informed choices about their health and treatment plans.
Equally crucial is the role of healthcare professionals in guiding patients through these choices. Open and honest communication with doctors or therapists can ensure that clients receive tailored advice concerning alcohol consumption alongside their treatment regimen. Ultimately, the decision to consume alcohol while on antidepressants should not be taken lightly. Being well-informed about the potential impacts ensures that individuals can navigate their mental health journey effectively and sustain their overall well-being. By prioritizing education and professional guidance, individuals can better manage their treatment and lead healthier, more balanced lives.

